Helping Medical Professionals During COVID-19
The level of risk in patient care today is higher than most providers ever considered when choosing medicine as a profession. The war metaphors being used in the Covid-19 fight aptly fit the threat doctors are experiencing. To emotionally bolster staff and lessen residual trauma, medical leaders and front line providers can benefit from applying well refined military crisis leadership strategies.
I recently discussed five essential components with fellow psychiatrist and former Navy Captain, Paul Hammer, MD.
MISSION: The leader makes meaning for the teams’ mission, discussing why their undertaking is important and why each role is crucial.
LEADERSHIP TRUST: The team trusts their leader prioritizes their safe passage through the battle.
SPECIFICITY OF SUCCESS: Success is concretely defined and only encompasses areas that they can control.
POST MISSION DEBRIEF: After the battle, leaders recognize all that was accomplished in spite of the challenges.
SUPPORTIVE FOLLOWUP: Availability of on-call support for emotions that arise after the group disperses.
Healthcare Applications:
For leaders wanting to provide the best outcome for their team and support for their members, lessons from the military include:
- Communicate the why behind what you are doing. This builds confidence and commitment. Speak about why you choose to be at the hospital, in spite of the risk and anxiety it brings; put into words what you value about being there, what your presence means to patients and others depending on your care. Share what each team member brings to the team, what would be missing if any one of them was not there.
- Team leaders can build trust by checking staffs' fatigue, tension and fears as they work. To empower team members, point out their capabilities. Help problem solve by brainstorming solutions together. Encourage time out when you see signs of exhaustion.
- Project calm to bring everyone’s emotional activation down. Let the team know you are a port in the storm. Show you are in this together. Be honest about the difficult situations you face; not being able to provide optimal care, being frustrated by policies or people, feeling the systems has let them or their patients down. Empathize they may face situations with no good answers. Model that this is a time to stop using shame and blame.
- Build psychological resilience during times of high patient death and limited resources by applying a mindset of success measured in maintaining focus on what they can control in spite of all they cannot.
- Remind staff to set realistic expectations for themselves, understanding they are working in never before experienced and ever changing circumstance with people who are tired and anxious. This is especially important in healthcare settings where providers are notoriously self-critical about problems they can’t overcome.
- Give them support to put aside negative thoughts to keep focused and moving ahead. When you check in, expand your usual question from, “How are you doing, everything ok?” to “What is most stressful/challenging/difficult right now?” and “What could you use help with?”
- Post-shift, acknowledge the reality of what the circumstances prevented their doing, the loss and grief they faced. Recognize their strengths in carrying on in spite of this.
Cathy Lanteri, MD, FAPA

Cathy Lanteri, MD, brings a distinctive breadth of expertise in human behavior, leadership, and communications to help healthcare leaders and front line clinicians find clarity, cohesion, and action in the midst of enormous pressure. As an executive coach and consult with The Leadership Development Group she helps clients to strategize and strengthen their effectiveness. Dr. Lanteri’s coaching draws from working with healthcare and medical industry leaders as well as 25 years of medical experience - at major Harvard teaching hospitals, developing a community satellite clinic, and in private practice. She combines this with knowledge of human dynamics and neurobehavior to heighten leadership performance.
Outside of her coaching and medical practice, Dr. Lanteri serves on multiple committees at Massachusetts Medical Society and is on the Board of Directors for Physicians Insurance Agency of Massachusetts. She speaks nationally on career leadership, communications, and burnout prevention. She is on the advisory board of the Physician Coaching Institute, where she developed educational programing for graduate coaches.
Paul Hammer, MD; FAPA; CAPT, MC, USN(RET)
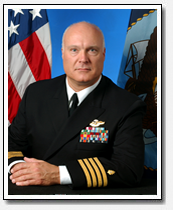 Dr. Hammer is a staff psychiatrist at Island Hospital, Anacortes, Washington. He has worked extensively with military organizations and is past president of the Academy of Organizational and Occupational Psychiatry. Dr. Hammer served 2 tours in Iraq and held the positions of Director of the Department of Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury as well as Director of the Naval Center for Combat and Operational Stress Control in San Diego.
Dr. Hammer is a staff psychiatrist at Island Hospital, Anacortes, Washington. He has worked extensively with military organizations and is past president of the Academy of Organizational and Occupational Psychiatry. Dr. Hammer served 2 tours in Iraq and held the positions of Director of the Department of Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury as well as Director of the Naval Center for Combat and Operational Stress Control in San Diego.



