In this timely article, we are sharing the unique and triumphant story of how Northeast Georgia Health System (NGHS) cultivated physician engagement despite the myriad challenges of COVID-19 by leveraging our Applied Physician Leadership Academy (APLA).
What was the State of Mind for Physicians Serving on the Frontlines of the COVID-19 Pandemic at Northeast Georgia Health System
Like so many healthcare providers, during the onset of the pandemic, the physicians at NGHS were feeling overwhelmed, overworked, and burned out. While three out of four surgeons at NGHS were forced to cancel elective surgery, cardiothoracic surgeons and the like had no choice but to continue doing their jobs through uncertainty while risking their lives in the process.
“We come in and feel like we are serving in a war. You see your phone starts buzzing at 6 am and it doesn't stop till 10 pm,” says Deepak Aggarwal, MD, Chief of Medical Staff at NGHS.
The pandemic caused the leadership at NGHS to restructure its organizational processes. They doubled the number of ICU beds and added about 300 medical beds to meet the increasing demands of patients sick with COVID-19. The leaders at NGHS realized that physician leadership, among other things, was a viable solution to addressing the challenges brought on by the pandemic.
Developing a Physician Leadership Program in the Midst of a Crisis
The first step NGHS took to kickstart APLA was through our organizational priority assessment (OPA). The OPA includes interviews with key stakeholders and robust data analysis. We interviewed 10 business leaders including the CEO, COO, and various senior physician leaders in the organization. During these interviews, we sought to understand and engage with leaders and provide an opportunity to allow them to share their hopes and concerns as well as socialize the program. Questions we asked included:
- What are NGHS’ most important strategic priorities for the next 1-5 years?
- Which skills need to be developed to position NGHS physician leaders to meet these challenges?
- What are the most important challenges to be solved to enhance the relationship between physicians and administrators?
These questions served as a way to surface common leadership themes and share challenges and frustrations from both administrative and physician leaders. After collecting this information, we then analyzed the results to inform the customized design of APLA for NGHS including:
- How to measure program success
- What barriers we needed to watch out for
- What the content of the learning sessions would be
- The structure and design of the physician coaching program
- Organizational challenges that could be used as the basis for physician Action Learning
"NGHS really does this program right — in the sense that it is created through a collaborative relationship between executives and physician leaders. From the needs assessment to the design team, to the implementation of the program itself, both voices had influence over the design and delivery."
— Tara Satlow, PhD, Senior Vice President, Client Solutions, TLD Group
As is standard in all TLD Group leadership programs, we also assembled a small design team comprised of TLD Group team members, NGHS executives, and NGHS senior physician leaders. This group met weekly to discuss:
- Program Updates and Customization- where each physician was in the coaching process, leadership themes emerging through coaching, upcoming didactic learning modules
- Real-time Program Feedback- Participant feedback on didactic learning sessions, challenges faced by the action learning teams, TLD Group faculty impressions, and feedback on their experience working with the participants
- Organizational Updates- What was currently going on within NGHS as a system, COVID-19 updates, and new organizational initiatives
“Having the ability to provide input almost on the fly every week really created a very personalized experience for us. And we created presentations and solutions that were unique to us. And that was a key component in making this whole thing work.”
— John Clifton Hastings, MD, Recent Past Chief of Staff, NGHS
How APLA Was Designed and Cohort Selection
Our programs utilize the 70/20/10 leadership development framework, based on the adult learning theory of Eichinger and Lombardo. Their research indicates that the most effective way to learn is to utilize a variety of learning modalities as follows: 10% of learning should incorporate interactive training courses focused on the development of specific leadership skills and competencies, 20% of learning should be through assessment and coaching, and 70% of learning should entail hands-on experiential learning in which learning is directly applied and leadership competencies are developed through work on real business problems.
When it comes to selecting the right cohort, we started by prioritizing a mix of senior physician leaders and high-performing leaders. We also placed a focus on the diversity of backgrounds, skills, and perspectives. There were three other areas that we took into account, as well:
- Low physician engagement scores – to engage those leaders so we could better understand why their engagement was low and then involve them in creating a solution for the organization.
- Individuals who could potentially be of assistance to us when we established our goals for the coming year.
- Individuals who were serving key positions but had very little management or leadership training.
From here, participants were assigned to coaches based on personality, experience, development goals, and other key factors.
Potential Barriers to Success
One of the primary barriers to success was severe time constraints due to the pandemic. Even under normal circumstances, undergoing a leadership development program requires a substantial time commitment. But, the pandemic-related restrictions on physician time as well as safety concerns to prevent further spread of COVID-19 were certainly things that we took into consideration as we designed the program. Thus, to satisfy the program requirements and those of the cohort, we created a hybrid design incorporating both in-person and virtual sessions.
"Implementing a large-scale leadership development program in the midst of a global pandemic is no easy feat. Lucky for us, agility and the ability to customize our solutions to meet the specific needs of our clients are key strengths of TLD Group. Because we're so accustomed to flexing our designs to client needs, flexing to meet the environmental constraints created by the COVID-19 pandemic was just a natural extension for us.”
— Tracy Duberman, Ph.D., President, and CEO, TLD Group
The Top 3 Strategic Imperatives That Needed to be Addressed in order for NGHS to Succeed
- NGHS needed physician leadership to be involved with larger strategic system development goals particularly as they relate to population health or service line development.
- NGHS required physician engagement and leadership involvement on the day-to-day issues, the goals relative to performance in the safety arena and in quality, how to deal with issues of readmission, and the relationships that physicians have with the nursing staff.
- Merging disparate silos into a group functioning together to drive positive change and organizational outcomes.
APLA Program Design Framework
Each of the 30 participants were assigned to a coach and began their engagements with an in-depth interview with their coach and an emotional intelligence assessment — the EQI 2.0. Each received feedback and development planning followed by 6 months of 1:1 executive coaching. Throughout the program, participants also participated in custom-designed learning sessions rooted in the following leadership competencies:
- Leading Self: Capitalizing on emotional intelligence to effectively lead
- Leading for Results: Building acumen and financial literacy — how to contribute to operational success
- Leading Change: Population health — collaborating and building partnerships
- Leading Others: Adaptive leadership — leading effectively in groups and teams
Each session culminated in a specific NGHS call-to-action which focused on tying the learning back to NGHS’ organizational goals.
Participants collaboratively put their learnings to the test through a facilitated action learning process. Working in four project teams (of 5-6 people each), the participants took on projects linked to strategic organizational priorities- such as enhancing dyad partnerships to drive engagement and performance metrics- while developing their leadership skills. The action learning process culminated in a Capstone presentation event where the participants presented their recommendations to NGHS executive leadership. This created a win-win scenario in which physicians were able to strengthen their leadership skills in real-time and be part of a system-wide solution.
Cultivating Physician Engagement During the Pandemic: The Results
We had great success with this program as evidenced by the data that we collected through pre and post-assessments and evaluation surveys. At the beginning and end of the program, all participants completed an assessment based on the metrics in the graphic below. We saw significant improvements across all four leadership clusters.
Overall, the program feedback was fantastic. See the chart below depicting participants’ feedback on the program’s components and effectiveness.
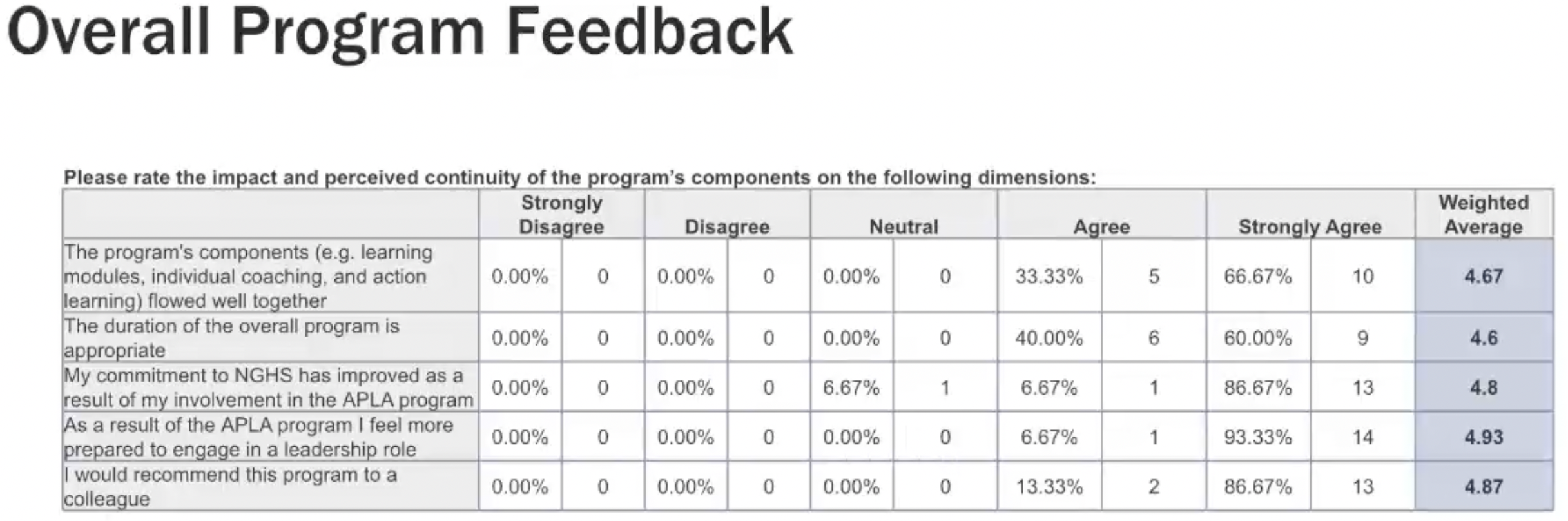
100% of participants agree that as a result of APLA, they feel better prepared to engage in a leadership role and feel a stronger commitment to NGHS. When asked about his experience with the APLA program, John Clifton Hastings, MD, Recent Past Chief of Staff, NGHS, said, “It brought people together from disparate areas of the system, and really created a cohesive group. You can see that in how we manage COVID and our use of resources. You can see it in terms of our medical executive committee because we have merged all of our medical staff. And that's made a difference as well. So we have people that are leaning in to make this successful.”
Key Takeaways
- Leadership development programming is a way to stay focused on strategy and move forward through a crisis.
- Development activities such as coaching can help physician leaders feel understood and empowered through a crisis.
- In-person connection outside of clinical work is a powerful engagement strategy for those on the front lines.
- Investment in physician leadership development enhances organizational commitment.
What’s Next for NGHS?
NGHS has given the first cohort of participants the opportunity to continue with their coaching. Several of the physician leaders who participated in the program have moved into more advanced medical director roles. As a demonstration of their continued commitment to this important work, NGHS leadership has created a medical director position for physician leadership development.
“We are proud to be kicking off our second cohort of the Applied Physician Leadership Academy this year, ensuring a strong pipeline of developed physician leaders will be able to support the organization’s continued success,” said Michael Covert, COO, NGHS.
Final Thoughts
Leadership development programs are impactful for cohorts of physician leaders, particularly at a time of crisis. Ultimately, leadership development programs provide a way to stay focused on strategy and move forward through a crisis with targeted and intentional support, connection, and development which serves to empower physician leaders through the challenges.
Hear from the leaders at NGHS as they discuss how an investment in physician leadership development enhances organizational commitment in the webinar, Cultivating Physician Engagement During the Pandemic. Watch the webinar recording here.
Our customized leadership academies are designed to build the required capabilities of specific leadership cohorts. Graduates become leaders who can inspire trust and engagement, define a clear and compelling purpose, and unleash the talents and energy of their teams.
Contact us today to learn more about how our leadership academies can improve dyad leadership through physician leadership development.



